
Eye rubbing is a habit many people engage in, often without much thought. It might temporarily relieve itching or dryness, but frequent and vigorous eye rubbing can have serious consequences, particularly for the cornea. One significant risk associated with this habit is the development and progression of keratoconus, a progressive eye disease that can lead to severe vision problems. In this post, we’ll delve into the relationship between eye rubbing and keratoconus, the symptoms and treatment options, and strategies to protect your eyes from harm.
What is Keratoconus?
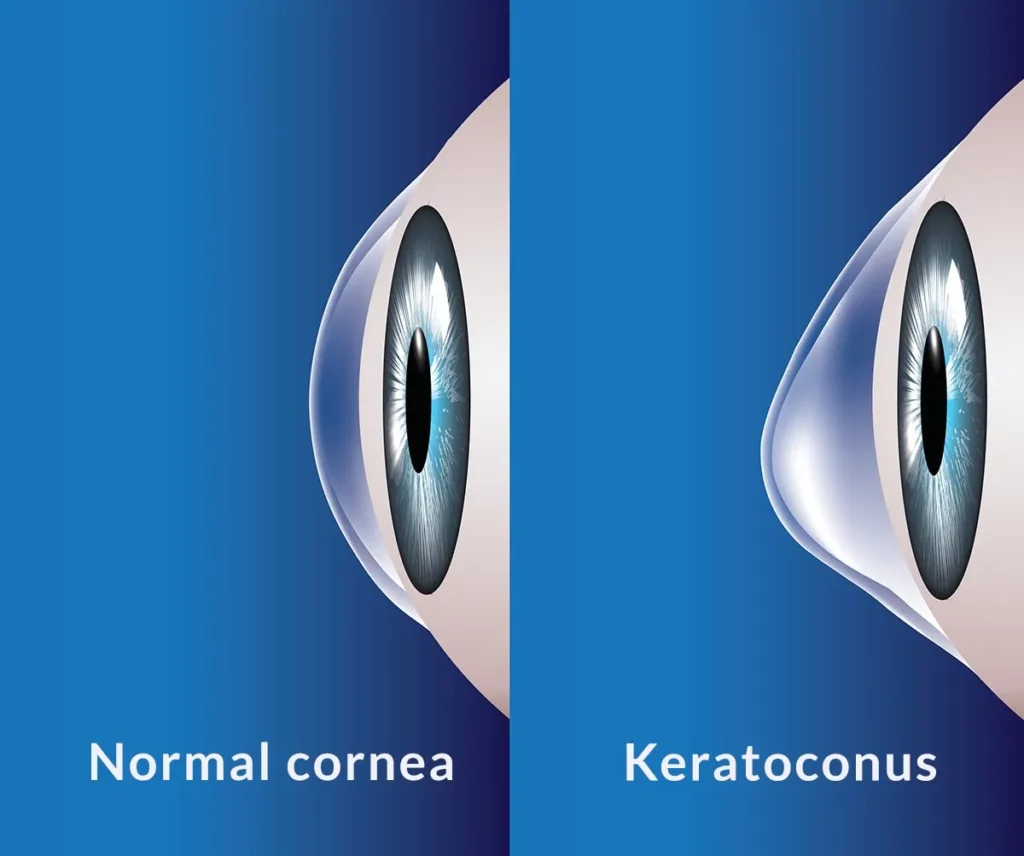
Keratoconus comes from the Greek kerato, meaning cornea, and conus, meaning cone. It is a condition in which the cornea – the clear, dome-shaped front surface of the eye – gradually thins and bulges into a cone-like shape. This abnormal shape distorts vision, making it difficult to see clearly, even with contacts or glasses. Contacts and glasses only correct lower-order aberrations like nearsightedness, farsightedness, and astigmatism. The abnormal corneas in keratoconus generate higher-order aberrations, leading to haloes, glare, image doubling, and blurriness that cannot be corrected with standard contacts or glasses.
Keratoconus is uncommon– affecting 1 in 700 Americans – but early diagnosis is critical to halt disease progression. In severe stages, the cornea can become so thin and irregular that a corneal transplant is warranted.
Causes and Risk Factors for Keratoconus
The cornea is predominately comprised of highly organized collagen bundles, granting the cornea strength, flexibility, and clarity. Keratoconus results when the connections between these collagen bundles are damaged from a combination of genetic factors and mechanical trauma – i.e., eye rubbing. Below is a list of risk factors for keratoconus, broken into one of two categories: conditions associated with increased eye rubbing and conditions associated with weak collagen.
Eye Rubbing
- Eye allergies
- Retinitis pigmentosa
- Down syndrome
Weak collagen
- Sleep apnea
- Connective tissue disorders
- Floppy eyelid syndrome
- Hormonal changes of pregnancy
- Hypothyroidism
Family history, which manifests as a combination of these two categories, is also a key risk factor for keratoconus.
The Link Between Eye Rubbing and Keratoconus
Several studies have shown a strong association between chronic eye rubbing and the development and progression of keratoconus. In fact, a popular dogma amongst ophthalmologists is, “No rub, no cone,” suggesting that keratoconus will not develop without eye rubbing, regardless of one’s genetic risk factors.
The purported mechanism is that mechanical trauma from eye rubbing causes damage to the connections between the collagen fibrils in our cornea. Enough of such damage will weaken the cornea’s ability to resist the outward-pushing force from pressure inside the eye. This causes the cornea to bulge forward, becoming thinner and steeper. Unfortunately, these changes are irreversible, so early detection and treatment are essential to prevent further progression.
Symptoms of Keratoconus
Keratoconus typically affects both eyes, though the severity can vary between them. The symptoms usually start in the late teens to early twenties and may include:

- Blurred or Distorted Vision: The cornea’s irregular shape causes light to scatter as it enters the eye, leading to blurry or distorted vision.
- Increased Sensitivity to Light and Glare: This is especially noticeable when driving at night.
- Frequent Changes in Eyeglass Prescriptions: As the cornea continues to change shape, new prescriptions may be needed more often.
- Difficulty Seeing at Night: Night vision can be particularly affected, making activities like driving challenging.
- Double Vision in One Eye: Known as monocular diplopia, this occurs when the cornea’s irregular shape causes multiple images to form on the retina.
Diagnosing Keratoconus
Keratoconus is diagnosed through a comprehensive eye examination from a trusted eye care professional. The most important tool in my box to diagnose keratoconus is my Pentacam, which is a corneal tomographer. Corneal tomographers use Scheimpflug cameras that take a rapid series of images and reconstruct a highly detailed 3D model of your cornea. The Pentacam’s software then compares your cornea to a normative database, generating a myriad of data points.
A skilled optometrist or ophthalmologist interprets this data to diagnose a host of corneal abnormalities, including keratoconus. Important hallmarks of keratoconus detected by the Pentacam include corneal thinning, corneal steepening, irregular astigmatism, and outward bulging of the inner and outer surfaces of the cornea.
I obtain a Pentacam for every LASIK evaluation to know whether the patient’s cornea is regular enough to undergo laser eye surgery safely.
Treatment Options for Keratoconus
The treatment of keratoconus depends on the severity of the condition:
- Cessation of Eye Rubbing: This is the most crucial intervention to preserve vision in patients with keratoconus.
- Eyeglasses or Soft Contact Lenses: In the early stages, vision can often be corrected with glasses or soft contact lenses.
- Rigid Gas Permeable (RGP) Contact Lenses: As keratoconus progresses, RGP lenses can provide better vision correction by creating a smooth refractive surface on the irregular cornea.
- Scleral Lenses: These larger lenses vault over the entire cornea, providing comfort and improved vision for those with advanced keratoconus.
- Corneal Cross-Linking: A minimally invasive procedure that strengthens the corneal tissue to halt the progression of keratoconus. This involves applying riboflavin (vitamin B2) eye drops and exposing the cornea to ultraviolet (UV) light.
- Intacs: Small, clear, plastic inserts placed within the cornea to flatten its cone shape and improve vision.
- Corneal Transplant: In severe cases where other treatments are ineffective, a corneal transplant may be necessary. This involves replacing the damaged cornea with healthy donor tissue.
Preventing Keratoconus: Breaking the Eye-Rubbing Habit
Years before I was born, my grandfather (rest in peace) stopped cigarette smoking cold turkey. He helped kick the habit by chewing gum every time he had a craving. I still associate Wrigley’s Juicy Fruit with my Pop Pops. My recommendation to stop eye rubbing is to be like Pop Pops and replace your habit with a new one: every time you feel the urge to rub, apply an artificial tear instead.
Below are a few additional strategies to help you stop eye rubbing:
- Identify Triggers: Understand what prompts you to rub your eyes, such as allergies, dry eyes, or fatigue.
- Manage Allergies: Use antihistamines and keep your environment clean to reduce allergens that cause eye itching.
- Use Artificial Tears: Lubricating eye drops can soothe dry and itchy eyes without the need to rub.
- Practice Good Hygiene: Wash your hands frequently and avoid touching your face to minimize the risk of transferring irritants to your eyes.
- Blink Regularly: Make a conscious effort to blink more often, especially when using screens, to keep your eyes moist.
Conclusion
While eye rubbing may seem like a harmless way to relieve irritation or fatigue, it can have severe consequences for your eye health, particularly in contributing to the development and progression of keratoconus. By understanding the risks and adopting healthier habits, you can protect your eyes and maintain better vision. If you experience symptoms of keratoconus, seek professional eye care to receive a proper diagnosis and explore the most suitable treatment options.
Thanks for reading,
Jonathan Corsini, MD


